Varicocele
Numerous studies show that presence of varicocele leads to impaired testicular development.
There are mainly 3 theories suggested in development of varicocele. These are anatomical differences between the right and left testicular veins, reflux (backflow) of the blood to the vein, and partial obstruction of the testicular veins.
Prevalence and Mechanism for Formation of Varicocele
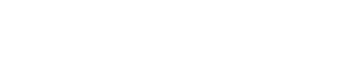
Defined as the abnormal dilatation of the veins that are responsible for venous return from the testicles, the term varicocele was originally coined by Curling in 1843. Varicocele is the most common treatable pathology of the male infertility.
Studies conducted show that varicocele can occur in 15% of men in general and 40% of men seeking medical help for infertility. According to the Guidelines of the European Association of Urology, varicocele is found in 12% of adult males whereas it is detected in 26% of patients who have impaired sperm values.
It is more common in the left testicle than the right testicle. The frequency of occurrence of varicocele in the left testicle alone is 90% whereas the frequency for the right testicle alone is relatively low, which is around 2%.
There are mainly 3 theories suggested in development of varicocele. These are anatomical differences between the right and left testicular veins, reflux (backflow) of the blood to the vein, and partial obstruction of the testicular veins.
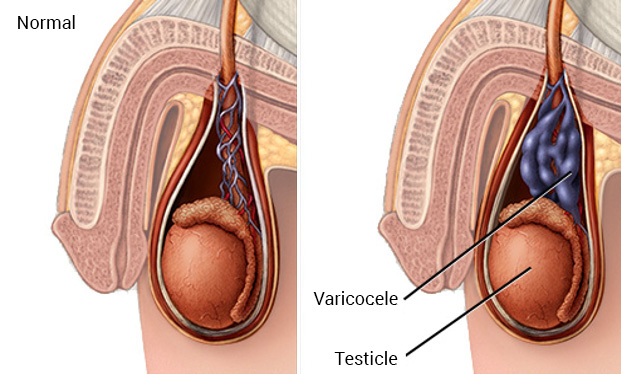
Anatomical differences between the right and left testicular veins:
Whereas right testicular vein attaches to the vena cava, this is completely different for the left testicle. The left testicular vein drains into the left renal vein at a straight angle. The left renal vein drains into the vena cava inferior approximately 8-10 cm higher than the right testicular vein. Therefore, the left testicle is exposed to higher pressure and relatively slower blood flow than the right testicle.
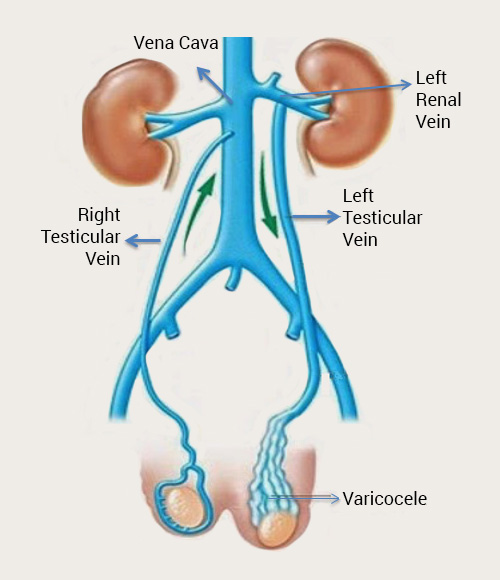
Reflux (backflow) to the vein
The lack or insufficiency of valves in the internal spermatic vein structure makes it easier for the blood to reflux. In a study conducted, venography of the veins of 659 patients with varicocele was performed, and no valves were detected in the testicular veins of 73% of the patients.
Partial obstruction of the testicular vein
Venous drainage of the testicles is obstructed as a result of compression of the left testicular vein that lies between the aorta and the artery that supplies blood the colons.
Impairment mechanisms of varicocele
Numerous studies show that presence of varicocele leads to impaired testicular development. There are various accepted theories to explain testicular impairment in the presence of varicocele.
Impairment caused by elevation of intratesticular temperature: This is the most commonly accepted theory of the varicocele.
Studies conducted have found out that mean intratesticular temperature of 30°C reaches 35-36°C in the presence of varicocele. The increase in temperature, which results from pooling of blood in the veins, leads to stoppage of sperm production. Anatomical structure of the scrotum and the network of veins ensures scrotal thermoregulation. The thin skin structure of the scrotum, absence of subcutaneous fatty tissue, and the muscle of the sac arranging the surface area ensure thermoregulation. The heat exchange between the testicular artery and the pampiniform venous plexus in its adjacency plays one of the main roles in temperature regulation of the testicles. High-temperature blood supplied from the abdominal aorta is cooled by the veins that carry lower-temperature blood. This mechanism works when the temperature of the blood in the vein is lower. ıt is believed that varicocele impairs this mechanism. In studies conducted, it has been observed that intratesticular temperature returns to normal levels after varicocele operation.
Another theory to explain the testicular impairment is the increasing intratesticular pressure. Increasing testicular pressure may lead to oncotic and hydrostatic pressure changes. As a result, the changing intracellular fluid balance affects conveyance of hormones. Additionally, it is suggested that impaired supply resulting from constant contraction of veins impacts sperm production.
The relationship of varicocele with hormones has been evidenced by studies conducted. Detrimental effects of varicocele include Leydig cell (the cells that produce testosterone) dysfunctions, impaired tubular structure, interstitial fibrosis and reduced sperm production. Leydig cell dysfunction might result in reduced testosterone levels. A study conducted show that intratesticular testosterone level must be minimum 20 ng/dl for healthy continuance of sperm production. The same study has found that intratesticular testosterone level is significantly lower in varicocele patients.
Looking at the other theories that try to explain the detrimental effects of varicocele on the testicles, it has been reported that the intratesticular hormonal level increasing as a result of the backflow from the kidney and the adrenal might affect the sperm production. It has been shown that reactive oxygen radicals caused by increasingly oxygen-free environment resulting from pooling of blood in the vein might lead to damages across all levels from impaired sperm production to sperm dysfunction.
Anti-Sperm Antibody (ASA) level, another accepted hypothesis, has been detected to be found in higher amounts in varicocele patients. Whereas ASA is detected in nearly 10% of the patients seeking medical help for infertility, ASA is detected in semen of 24-32% of the patients.
Effects of varicocele on testicles and sperm
In presence of varicocele, testicle volume might decrease or testicles might shrink abnormally, depending on the severity of varicocele, due to impairment mechanisms of varicocele. Reduction in testicular volume is more pronounced in patients at the advanced stage of varicocele.
Sperm test findings suggest that varicocele impairs sperm structures by lowering the sperm count and speed and result in infertility in patients. The semen analysis values required for fertility was published by the World Health Organization in 2010.
| Parameter | Defined Threshold |
| Semen volume (mL) | 1.5 (1.4-1.7) |
| Sperm concentration (106 per mL)n | 15 milyon/ml (12-16) |
| Total sperm count (106 per ejaculate) | 39 milyon /ml (33-46) |
| Total motility (%) | 40 (38-42) |
| Progressive motility % | 32 (31-34) |
| Viability (alive sperm cell) % | 58 (55-63) |
| Sperm morphology (normal structure % | 4 (3.0- 4.0) |
Varicocele Examination and Diagnosis
Varicocele basically diagnosed during clinical examination and confirmed with Color Doppler Ultrasonography (USG). “Subclinical varicocele” are those that are not detected during physical examination but detected through imaging techniques. Scrotal color Doppler USG, Venography, Thermography, and Scintigraphy are auxiliary imaging techniques that may be used.
Physical examination, which is significant in varicocele diagnosis, should be performed while the patient is standing and lying down in a warm room. The scrotum when lying down should be checked for asymmetry and vein enlargement. Spermatic cord, testicle size and consistency should be palpated when standing. Later, structure of the veins should be examined before and after Valsalva maneuver. The grading system developed by Dubin et al. in 1970 is used in classification of varicocele:
- Subclinical Varicocele: Not detectable during physical examination, and diagnosed with radiological techniques.
- Grade I Varicocele: Asymptomatic in resting state and detectable in straining state.
- Grade II Varicocele: Veins can be palpated while standing but they are not visible to the eye.
- Grade III Varicocele: Visible to the eye without the patient straining.
Radiological imaging techniques that can be used for diagnosis of varicocele:
- Scrotal ultrasonography:
Measurements are made while the patient is standing and lying down. The difference between the resting and straining states give information on the varicocele. Although vein diameters measured give an idea about the varicocele, there has not been a consensus on this method. According to an accepted view, examination of three or more veins in the network of veins and a vein diameter greater than 3 mm have been found to be sufficient for establishing subclinical varicocele diagnosis. According to another study, the varicocele diagnosis can be established if the difference in vein diameters is greater than 1 mm between the resting and straining phases. - Color Doppler USG:
Varicocele can be diagnosed if reflux is detected in the testicular vein before and after the straining maneuver. The reflux measured is categorized as short-term reflux if it lasts shorter than 1 second, intermittent if 1-2 seconds, and permanent or continuous if longer than 2 seconds. It has been determined that short-term and intermittent refluxes are physiological whereas permanent or continuous reflux is significant in diagnosis of varicocele. - Venography:
The use of venography in diagnosis of varicocele was first described by Ahlberg in 1966. Whereas it is accepted as the gold standard in diagnosis of varicocele, it is no longer widely used since it is a long and invasive procedure. It can be applied for examining the drainage of the vein in patients who will undergo sclerotherapy or embolization treatment and recurrent varicocele treatment. - Thermography:
Scrotal temperature is 3-4°C lower than the body temperature in healthy individuals. Studies conducted demonstrate that testicular temperature increases in varicocele patients as a result of increased reflux into the testicle. Varicocele is diagnosed by determining the temperature increase with measurements performed with high-sensitivity cameras or temperature-sensitive thermostrips. A difference of 1°C between both testicles is sufficient for establishing varicocele diagnosis. - Scintigraphy:
Varicocele can be diagnosed if the pooling of blood in testicular veins is viewed with Tc99 (Technetium 99m). Popular in the early 1980s, this technique has lost its significance today since it is time-consuming and has low sensitivity.
Who should receive varicocele treatment?
Infertility is the most prominent cause of varicocele treatment. According to the infertility committee of the American Urological Association, the following conditions should be met before varicocele treatment:
- Female partner has normal fertility or a correctible infertility;
- Varicocele is revealed during physical examination or viewed with USG, if varicocele is suspected;
- Infertility of the married couple has been documented with the necessary tests;
- The patient has one or more abnormal semen parameters in his spermiogram.
Who should receive varicocele surgery?
- Male patients who have abnormal sperm values, who are single, or who are married and planning on having children later are candidate for varicocelectomy operation.
- Patients seeking medical help due to pain caused by varicocele describe a blunt pain that spreads to the inguinal area. This pain is described as a sensation of straining or heaviness by patients. Firstly, conservative approaches should be adopted, such as scrotal elevation, medication with analgesics, and evaluation of pain caused by other conditions. Surgical treatment should be offered to patients who do not respond to conservative approaches. Studies conducted show that pain is significantly relieved with varicocelectomy operation. However, it should be noted that the operation also has a placebo effect on patients.
- Many clinicians consider low testosterone level or reduced male hormone level in follow-up as an indication for operation. Studies conducted demonstrate the detrimental effects of varicocele on Leydig cells and varicocele operation corrects this pathology.
- Effect of varicocele operation on infertility during adolescence has yet to be demonstrated clearly. Varicocele operation is indicated in adolescents if a volumetric difference of 10-20% (nearly 2 cc) is present between both testicles.
Treatment methods for varicocele
Varicocelectomy is the most commonly performed surgical treatment for male infertility. It first started to be performed in early 1900s by means of open scrotal surgeries. Since arteries cannot be identified during this surgical technique that involves total removal of varicose veins, the risk of testicular impairment and atrophy is high. Therefore, a surgeon named Palomo developed a technique in 1949, in which veins are tied in the inguinal ring, the area where the branching of arteries and veins is little. However, rates of recurrence were found to be higher in this technique since gubernaculum and external spermatic vein could not be controlled.
Laparoscopic varicocelectomy is a technique that applies the Palomo technique with a retroperitoneal approach. The artery and the vein could be detected better thanks to the magnified images provided with laparoscopy. The rate of recurrence is 15-20% compared to open Palomo technique. It has lost its popularity today due to high costs and risk of major organ injuries.
Inguinal varicocelectomy operation was first described by Ivanissevich in 1960. An incision in the groin at the level of the inguinal canal allows easy access to the spermatic cord and the testicle and examination of all venous structures. Microscopic varicocelectomy operation was first described by Marmar et al. in 1985. In this approach, which is described to be subinguinal, the patient heals fast since the inguinal canal is not opened. However, the operation could become complicated since branching of the arteries and veins is high at this level. It can be preferred in obese patients and patients who have undergone inguinal surgery.
Sclerotherapy is another treatment method for varicocele in form of occlusion of the internal spermatic vein. A recurrence rate of 4-11% is reported. The main reason of recurrence is the inability to close the veins with a plug.
Impacts of varicocele on infertility
It is known that varicocelectomy leads to significantly improved results in the sperm tests of 60-80% of patients. Rate of pregnancy range between 20% and 60%. In a study by Goldstein et al., rate of pregnancy was reported as 69%. A study by Marmar et al. showed that rate of pregnancy increased by 2.8 times with varicocelectomy in patients who had varicocele and had at least one impaired parameter of sperm. It was reported that, as a result of the varicocelectomy operations performed on varicocele patients who were azoospermic, i.e. who had no sperms, semen analysis results indicated sperm by nearly 60%.
Microscopic varicocelectomy is the most prominent technique among the surgical treatments available for varicocele. The pregnancy rates achieved with microscopic varicocelectomy operation have been found to be higher than other conventional techniques. Recurrence and hydrocele rates have also been found lower than other techniques.
Possible complications of varicocele operation
Post-varicocele operation complications might include recurrence, hydrocele, testicular atrophy, and nerve and seminal duct impairments. Table below shows the frequency of the complications according to 2014 Guidelines of the European Association of Urology.
| TREATMENT | RECURRENCE% | FREQUENCY OF COMPLICATION |
| Antegrade sclerotherapy | 9 | 0.3-2.2%: Reduction in testicular structure, scrotal blood pooling, epididymitis, left flank erythema |
| Retrograde sclerotherapy | 9,8 | Contrast agent reaction, pain in the left side, venous damage, thrombophlebitis |
| Retrograde embolization | 3,8-10 | Pain caused by thrombophlebitis, hematoma, infection, radiological complications |
| Scrotal varicocelectomy | * | Testicular atrophy, devascularization and gangrene caused by arterial injury, hydrocele, hematoma |
| Inguinal varicocelectomy | 13,3 | Overlooking one branch of the testicular vein |
| High ligation (Palomo) | 29 | Hydrocele (5-10%) |
| Microscopic inguinal/subinguinal varicocelectomy | 0,8-4 | Hydrocele <1%, scrotal hematoma, arterial damage |
| Laparoscopic varicocelectomy | 3-7 | Testicular artery and lymphatic vessel damage; intestinal vascular and nerve damage; pulmonary embolism; peritonitis; bleeding |
Book an Appointment with Dr. Fatih Atug
Cantact Dr. Fatih Atug
Fatih Atug, M.D.
Urologist and Robotic Surgery Specialist
hidden +90 212 234 5958
hidden +90 532 234 5504
hidden info@fatihatugmd.com
hidden Harbiye Mahallesi, Maçka Caddesi,
Bahriye Apt. No:13 D: 3
Şişli / İSTANBUL
 |
 |
 |