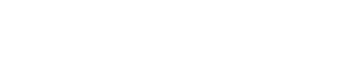
Benign Prostatic Hyperplasia (BPH)
Prostate gland starts gradually enlarging after the age of 40.
This is called BPH (benign prostatic hyperplasia), a medical term used to describe benign prostate enlargement.
Function and structure of prostate
Prostate gland is located right below the bladder in men, surrounding the tube called urethra that discharges urine from the bladder. In an adult men, the prostate gland weighs about 25-30 grams. The primary role of the prostate is to produce the seminal fluid and help discharge of this fluid during ejaculation.
Prostate gland starts gradually enlarging after the age of 40. In particular, the inside of the prostate may enlarge, and the prostate gland, which is normally about the size of a chestnut, may become as large as an apple or even an orange. This is called BPH (benign prostatic hyperplasia), a medical term used to describe benign prostate enlargement.
Studies conducted report that benign prostatic hyperplasia occur in 50% of men aged over 60 and 90% of men aged over 80. BPH and prostate cancer are different diseases. Whereas BPH does not cause prostate cancer, both can occur concurrently.
As the prostate enlarges, it blocks the urethra, preventing the flow of urine. As the disease progresses, patients start experiencing symptoms related to urination, depending on the degree of obstruction. Symptoms of patients are evaluated in 2 main groups:
Obstructive symptoms:
- Reduced flow and weak stream of urine
- Difficulty starting urination
- Intermittent urination
- Dribbling at the end of urination
- Feeling the bladder is not completely empty
- Blood in the urine
Irritative symptoms:
- Frequent urination (day and night)
- Urgent need of urination
- Urinary leakage in case of urgency
- Burning and stinging during urination
Sometimes, the urethra gets completely blocked due to BPH and the patient can suddenly become unable to urinate. It may be necessary to insert a catheter to the bladder of these patients.
Enlarged prostate is not a significant finding on its own in BPH. Aside from the enlargement, development of symptoms in the patient, increase in the severity of the symptoms and the complications in the urinary tract caused by the enlargement are also among the factors that reveal the significance of the disease.
Complications in the urinary tract caused by BPH are as follows:
- Sudden inability to urinate: The urinary tract is completely obstructed and the patient is unable to urinate. This is also accompanied by a severe pain in the lower abdomen. A catheter should be inserted into the urinary tract in order to drain the urine in the bladder.
- Urinary tract infection: Obstruction of the urinary tract may result in the infection of the bladder. If it occurs, the patient may experience severe burning sensation during urination and high fever.
- Bladder damage: A bladder that has not emptied completely due to the prostate blocking the urinary tract can stretch and weaken and lose its ability to contract in time. If the bladder has lost its ability to contract, this will result in urine residue to remain inside the bladder. This damage may not be reversed sometimes even with a surgery.
- Bladder stones: Bladder stones are caused by sedimentation of the infection and minerals accumulating in the urine that remains in the bladder due to obstruction of the bladder.
- Kidney damage: Bladder infections may affect kidneys. On the other hand, increased pressure due to the obstruction of the bladder and the bladder residue always remaining inside the bladder may result in enlargement and dysfunction of the kidneys. Although rarely, some patients may develop renal insufficiency.
- Surgery is necessary for patients who have developed such complications.
Diagnosis of BPH
The cause of urination related symptoms in patients might not always be the enlargement of the prostate (such as diuretics, diabetes, urinary tract infections, bladder cancer, neurological disorders of the bladder, and urethral strictures, etc.). Therefore, the patient should be examined thoroughly before diagnosing them with benign prostate hyperplasia. The patient should always be asked about the medications they take, history of diabetes in their family, and any traumas previously experienced. Diabetic patients usually urinate more frequently. On the other hand, if a patient with early BPH is on antihistamines or decongestants for common cold, their symptoms will be even worse. Apart from that, the patients to be examined will probably be asked the following questions:
- What are your symptoms?
- How long have you been experiencing these symptoms?
- How frequently do you experience these symptoms?
- Have they gotten worse in time?
- Does anyone in your family have any prostate diseases (particularly, prostate cancer)?
- Are you taking any medication? If yes, what are those?
Digital Rectal Examination (DRE)
The urologist will examine the size, consistency and shape of the prostate. In case of a benign prostatic hyperplasia, the prostate will be relatively elastic and the increased volume can be detected. If any hardness is felt in the prostate, this is suggestive of cancer.
PSA test
The prostate gland produces an enzyme called Prostate-Specific Antigen (PSA), whose role is to liquefy the seminal fluid. A little amount of the PSA enters blood circulation. While high serum PSA occurs in BPH or Prostatitis – also known as prostate infection, it is also seen in prostate cancer. When age-specific PSA values are high (e.g. it should be less than 2 ng/ml in men aged under 50 and 2.5 ng/ml in men aged 50-60) and hardness is detected during digital rectal examination, prostate cancer should be ruled out. Not every increased PSA level suggests cancer; although, it is a fact that cancer may be present even when the PSA level is within reference range.
Urinalysis
In case of detected infection cells or blood cells in urinalysis, existence of another disease causing such symptoms should be ruled out (e.g. urinary system infections, urinary system stones, bladder tumors, etc.).
Urine flow rate
Normal maximum urine flow rate must be 15 ml per second, and the average flow rate must be 10 ml. Normal urination time is 30 seconds, which half a minute. If the prostate is blocking the urethra in BPH, such rates will be lower and the time of urination will be longer. The minimum amount of urine should be 150 ml for the test to be reliable.
Ultrasound examination
It is useful in obtaining information on the size of the prostate, its inner structure and the changes it has caused in the urinary system, using sound waves sent from the surface of the abdomen or the rectal route. Rectal ultrasound is also used for prostate biopsy.
Symptom score check:
This inquiry system called IPSS is useful in understanding the symptoms of the patients. It is also useful in understanding the effectiveness of the treatment during follow-up of patients after medical or surgical treatment.
PMR (Post-mictional residue) determination
It is detection of the amount of urine left in the bladder after urination. In general, it is performed with an ultrasound device called the “bladder scan”. A catheter is inserted into the urethra for a more reliable measurement; however, this method is uncomfortable for the patient.
Urodynamics; Pressure-Flow test:
When it is suspected that the symptoms related to urination are caused by prostate enlargement (particularly in young or very old patients; patients who do not have increased prostate volume), a urodynamics device is used to measure the bladder pressure and the flow rate and pressure in the urethra by means of a catheter inserted into the urethra. This way, it is understood whether the symptoms of the patient are caused by any deterioration in the contraction ability of the bladder.
Cystoscopy:
It is a procedure performed by inserting a device called cystoscope into the urethra under local anesthesia in order to understand how much the prostate blocks the urinary system and whether there is any other disease involving the urinary system.
Intravenous Urography or Computed Tomography
Aside from prostate enlargement, in case of presence of blood cells in the urine or a suspicion of urinary stone disease, it is used to obtain more detailed information on the kidneys and the urinary system by means of administering radiopaque material containing iodine intravenously or by means of thin-slice tomographic images.
*This procedure is not performed on those who have creatinine levels higher than normal.
Treatment for Benign Prostate Hyperplasia
A) Non-invasive treatments
Follow-up: Presence of BPH does not always necessitate treatment. A patient who does not have any difficulty urinating and any related signs and symptoms could be kept under surveillance if can be established during urological examination that the kidneys and the bladder are not damaged. The urologist prepares a follow-up program for the patient for visitation at the recommended intervals, the longest of which is one year.
Medication: When symptoms of BPH have started to disrupt the person’s daily activities and quality of life, treatment is recommended. Generally, the first option is medication.
5-Alfa reductase inhibitors: Finasteride (Prosterid®, Proscar®, Dilaprost®) and dutasteride (Avodart®) are examples to the medication. They function by inhibiting conversion of testosterone into dihydrotestosterone (DHT), the active form of testosterone. It is reported that, this way, they help shrinking of the prostate to some extent. Their side effects might include loss of libido, impotence, swelling and tenderness in breasts, and decrease in sperm count.
Alpha-blockers: These medications help enlarge the urethra by relaxing the smooth muscle structures in the bladder neck and the prostate. These medications are taken once a day. The most known medications include Alfuzosin (Xatral®), Doxazosin (Cardura®), Terazosin (Hytrin®), and Tamsulosin (Flomax®). Their side effects might include headache, dizziness, fatigue, weakness, and low blood pressure.
B) Minimally invasive treatments:
Prostatic Stent applications: Prostatic stents may be applied to patients who do not respond to medical treatments and require surgery but cannot be operated due to general health conditions. It is a spiral-shaped apparatus that is placed through a fine tube and enlarges the urethra every time it opens. Most commonly used stents include Urolume® and Memotherm®. Their advantages include no hospital stay, very little risk of bleeding, and quick application. Their main disadvantages might include that the stent is not placed well sometimes and might become dislodged and move, cause irritation and, as a result, frequent urination, urinary incontinence, and pain.
Transurethral Prostate Resection (TURP):
Transurethral Prostate Resection is the most commonly used method in surgical treatment of benign prostatic hyperplasia (BPH). In this method, after the patient is put under general anesthesia or lumbar (spinal or epidural) anesthesia, a special device called resectoscope is advanced through the urethra and the prostate tissues are cut using electric current. Continuous irrigation is necessary throughout this procedure during which a probe device with optical viewing capability sends the images of the patient’s insides to a monitor where the images are enlarged 10-12 times. The electric current is sent to the tissues with a semicircle wire called the “loop”, and while the prostate tissue is cut in strips, the loop stops the bleedings. The prostate tissues accumulating inside the bladder are later evacuated using a vacuum system. A cathether is inserted into the urethra after the operation, which is left there for 2 days.
The greatest advantages of transurethral prostate resection are the ability to remove the part of the prostate that obstructs the urinary tract and create a cavity and the ability to perform a pathological analysis of the tissues removed. Although rarely, bleeding might occur during or after the surgery, which mostly does not require blood transfusion. Urinary tract stricture might occur seldom, if ever, after the surgery.
Greenlight Laser for Enlarged Prostate
Laser has been increasingly used in many fields of medicine in recent years, and many types of laser have been used in prostate surgeries by now. Greenlight laser is the most commonly used laser method in surgeries. The KTP laser used in greenlight laser prostatectomy - also known as PVP (photoselective vaporization of the prostate) - creates a green light, which is why the method is called as the “Greenlight Prostatectomy”. The KTP laser is selectively absorbed by the prostate tissue; in other words, it has a selective feature for the prostate. The greenlight laser energy is in fact absorbed by the serum hemoglobin and evaporates the blood vessels along with the prostate tissue. This is why there is scarcely any bleeding during the procedure.
Application of the Greenlight Laser Operation
The operation may be performed under general anesthesia or lumbar anesthesia (administered with a needle into the lumbar region without putting the patient under general anesthesia). In high-risk patients, local anesthesia methods may also be adopted. A special device (cystoscope) is advanced through the urethra of the patient to view the bladder and the prostate, and the prostate is evaporated by the light beams irradiated by the laser probe guided in through the device. As a result of instant evaporation of the prostate tissue by the laser beams, a cavity is created, allowing easy flow of the urine. Since no tissue is removed for post-operation pathological analysis, all patients must have been examined thoroughly for prostate cancer before this procedure.
Greenlight Laser Operation

Advantages of Greenlight Laser
- The operation can be performed on patients taking blood thinners, such as Aspirin or Coumadin, without stopping the medication. Patients taking these medications, also known as anticoagulants, need to stop taking them prior to both open prostate surgeries and closed prostate surgeries like TUR-P due to risk of bleeding. In greenlight laser operation, though, there is no need to stop these medications. This is because the greenlight is absorbed by the serum hemoglobin and evaporates the blood vessels along with the prostate tissue. This is why there is scarcely any bleeding during the procedure.
- There is little or no bleeding. During greenlight laser operation, a coagulation zone forms below the evaporating part of the prostate. This is why there is almost no bleeding during and after the operation.
- Early removal of catheter: The catheter is removed earlier and length of stay in hospital is shorter in greenlight laser operation than other operations (24 hours).
- The length of stay in hospital is very short. Greenlight laser operation is performed as a one-day surgical operation in a lot of centers in the United States. The patient can be sent home in the evening of the same day.
- There is no risk of TURP syndrome. Isotonic solution is used during the greenlight operation; thus, the ‘TURP syndrome’, which occurs as a result of absorption of the fluids used during the TUR-P operations, is not experienced.
The greenlight laser operation was first started to be used in the early 2000s with 60-80 watt capacity devices. Recently, in parallel with the technological advancements, 120-watt models (HPS) have been developed and put in use. These devices, which are more powerful than the previous models, offer the advantage of evaporating more tissues in a shorter period of time. This way, patients who have larger prostates can be treated with laser.
Book an Appointment with Dr. Fatih Atug
Cantact Dr. Fatih Atug
Fatih Atug, M.D.
Urologist and Robotic Surgery Specialist
hidden +90 212 234 5958
hidden +90 532 234 5504
hidden info@fatihatugmd.com
hidden Harbiye Mahallesi, Maçka Caddesi,
Bahriye Apt. No:13 D: 3
Şişli / İSTANBUL
 |
 |
 |